Abscesses near the rectum—often called perianal or perirectal abscesses—are painful, pus-filled lumps that form when bacteria infect anal glands. Ignoring them can lead to complications, like fistulas (tunnels in tissue), deeper infection, and systemic illness. Recognizing symptoms and seeking care early is essential.
2 | How Abscesses Form
- Anal glands get blocked (by stool, debris).
- Bacterial growth—often E. coli or Bacteroides—leads to infection and pus.
- Pressure rises in tissue spaces causing swelling and intense pain.
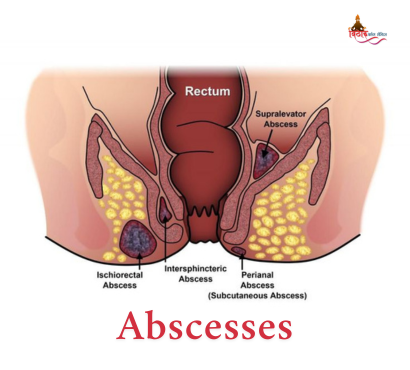
Abscesses are classified by location:
- Perianal – near the skin
- Ischioanal – deep into buttock
- Intersphincteric / supralevator – deep within pelvis
Equally, an untreated abscess may develop into an anal fistula—a tunnel connecting the gland to skin—seen in 40% of cases.
3 | Recognizing Symptoms
Key signs to watch for:
- Throbbing, severe pain, worsened when sitting or during bowel movements
- Visible lump or redness near the anus
- Fever, chills, general fatigue indicating infection
- Pus drainage, often with foul odour
- Constipation, difficulty urinating from pressure
Deep abscesses may not be visible but cause severe pain and fever.
4 | Diagnosis Steps
- History & examination—look for lumps, swelling, tenderness
- Digital rectal exam or anoscopy to assess deeper abscesses
- Imaging (ultrasound/CT/MRI) if not clearly visible, or when infection is deep
Blood tests and glucose checks screen for systemic infection and diabetes.
5 | Effective Treatment Strategies
A. Incision & Drainage (I&D)
- The primary treatment: drain under local or general anaesthesia.
- A small cut releases pus, relieves pain immediately. Antibiotics only if there’s fever or deeper infection (diabetes, immunosuppression).
B. Dressing & Sitz Baths
- Daily sitz baths (warm water) soothe pain and keep area clean.
- Loose clothing and soft dressings support healing.
C. Pain & Infection Control
- NSAIDs relieve pain and inflammation.
- If needed, antibiotics targeted to lab results.
D. Manage Bowel Movements
- Fiber-rich diet, fluids, and mild laxatives to prevent straining.
- Prompt attention to recurring pain and discharge.
E. Follow-Up & Fistula Detection
- Monitor for fistula signs (persistent discharge, recurrence).
- Further surgical intervention may be required if fistula develops.
6 | Risks of Delay
- Development of anal fistula in ~40% of untreated cases
- Spread of infection causing cellulitis or sepsis
- Recurrent abscesses, requiring multiple surgeries
- Chronic pain and ongoing discomfort
Timely treatment prevents serious complications.
7 | Prevention Tips
- Promptly treat infections or anal cutting/sores
- High fiber diet, hydration, good bathroom habits
- Manage chronic conditions like diabetes or Crohn’s
- Seek immediate care at first sign of red, painful lumps
8 | Patient Experience
Most patients experience significant improvement within 24 hours post-drainage. Complete healing typically occurs over 2–3 weeks. Deeper or complex cases involving fistulas may require specialist surgical care.
Perianal and rectal abscesses are treatable yet painful infections that require prompt attention. Awareness of warning signs—pain, swelling, fever—plus early drainage, hygiene, and medical care prevent complications like fistulas and sepsis. If painful lumps near your rectum appear, consult a professional promptly.
FAQ
Q1. Can a perianal abscess heal on its own?
Sometimes minor abscesses drain spontaneously, but most require professional incision and drainage to prevent recurrence or deeper infection.
Q2. Are antibiotics necessary?
Not always—antibiotics are reserved for systemic symptoms like fever, diabetes, or immune compromise. Drainage is key.
Q3. How long until pain and swelling subside?
Pain often lessens within a day after drainage, with notable healing in 1–2 weeks. Complete recovery may take 3 weeks with proper self-care.