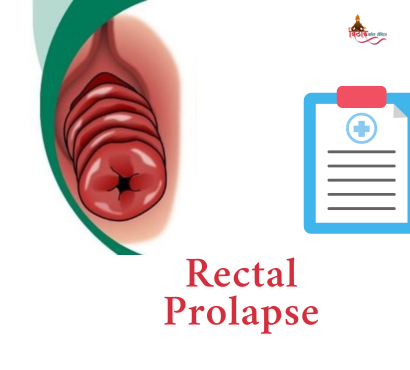
What Is Rectal Prolapse?
Rectal prolapse is a condition where part (or all) of the rectum protrudes through the anus, often during bowel movements.
- Complete prolapse means the full thickness of the rectal wall slides out.
- Mucosal (partial) prolapse involves only the inner lining.
- Internal prolapse (intussusception) occurs when the rectal wall telescopes inward without external visibility
How Common Is Rectal Prolapse?
- Affects roughly 2.5 in 100,000 adults annually
- Predominantly seen in women over 50, but can occur at any age
- Less frequent in children; often resolves without surgery in younger age groups
Signs & Symptoms
Key Warning Signs:
- Visible reddish lump protruding during straining
- Sensation of incomplete evacuation or rectal fullness
- Mucus or blood discharge
- Fecal incontinence or alternating constipation and diarrhea
Look out for persistent pressure after bowel movement or sudden pelvic heaviness.
What Causes Rectal Prolapse?
Rectal prolapse results from weakening of pelvic support structures—muscles, connective tissue, nerves—due to:
- Ageing, which naturally weakens muscle tone
- Chronic constipation or diarrhea, leading to straining
- Recurrent coughing or sneezing
- Childbirth, pelvic surgery, or spinal injuries
- Neurological conditions (MS, stroke) affecting nerve control
- Genetic factors, parasitic infections, cystic fibrosis in kids
Diagnosing Rectal Prolapse
A. Medical History & Physical Exam
Your doctor will evaluate symptoms, onset, and whether the prolapse reduces by itself or manual pushing.
B. Proctoscopic Exam
Includes digital rectal and straining maneuvers to visualise prolapse.
C. Additional Tests
- Defecography for internal prolapse
- Anorectal manometry, MRI or CT scans to assess severity and co-existing pelvic issues
First‑Line (Non‑Surgical) Management
Conservative measures may provide relief, particularly in early or mild cases:
- Dietary fibre & fluids to soften stool
- Avoid straining and use stool softeners
- Pelvic floor exercises (e.g., Kegels)
- Management of cough or respiratory issues
These methods may prevent progression but don’t remove existing prolapse in adults.
Why Surgery Is Often Necessary
In adults, rectal prolapse rarely resolves without intervention. Surgery aims to:
- Restore rectal position
- Repair pelvic support
- Prevent recurrence
- Reduce fecal incontinence and improve bowel control
Surgical Approaches
A. Abdominal (Rectopexy)
- Rectum is fixed to sacrum, often with mesh and laparoscopic or open methods
- Frequently combined with removal of redundant bowel in constipated patients
- High success (~95%) and low recurrence (~2–5%)
B. Perineal Procedures
- Altemeier (rectosigmoidectomy): Prolapsed bowel removed via anus
- Delorme procedure: Mucosal excision + muscle tightening
- Less invasive, suitable for older/frail patients, but higher recurrence (10–30%)
C. Minimally Invasive Options
- Laparoscopic, robotic rectopexy offer faster recovery
- STARR (for internal prolapse or rectocele) removes redundant tissue stapler-guided
Preparing for Surgery
- Bowel preparation and antibiotics are standard
- Choice of anesthesia (general or spinal) depends on patient health
- Discuss risks: bleeding, infection, constipation, incontinence, sexual dysfunction
Recovery & Aftercare
- Hospital stay: 1–5 days depending on technique
- Diet: Clear fluids → fibre-rich solid diet to avoid straining
- Activity: Gradual return over 4–6 weeks; avoid heavy lifting
- Exercises: Continue pelvic floor strengthening
- Follow-up: Monitor bowel habits, possible imaging if needed
Outcomes & Prevention of Recurrence
- Abdominal surgery offers durable results (<5% recurrence)
- Perineal approaches: recurrence up to 30% in 2–5 years
- Preventive measures include:
- Maintain soft stool
- Avoid constipation
- Regular pelvic floor exercise
- Manage chronic cough or weight issues
Rectal prolapse can significantly affect quality of life, causing discomfort, incontinence, and pain. In adults, surgery—either abdominal or perineal—is the definitive treatment and offers high success rates. Choosing the right procedure depends on your age, overall health, and recurrence risk. Early consultation and proper aftercare ensure the best results and prevent complications. If symptoms like anal protrusion, mucus, or fecal leakage persist, consult a specialist for diagnosis and to design the right treatment plan—even allowing normal life and comfort again.
FAQs
Q1 – Can rectal prolapse be managed without surgery?
In early internal or mucosal prolapse, lifestyle and pelvic exercises may help, but complete or recurrent prolapse in adults usually needs surgery
Q2 – Which surgery is best for older adults?
Perineal methods (Altemeier or Delorme) are safer under regional anesthesia but have higher recurrence. Abdominal rectopexy offers better long‑term results in healthier patients
Q3 – Could prolapse cause cancer?
Rectal prolapse itself is not cancerous. However, long-standing prolapse may cause ulcers or chronic irritation. Regular monitoring is crucial